

Reclaim Clarity in Your Care

We help patients untangle the confusion of healthcare — guiding you through every bill, benefit, and brave question with empathy and understanding.
Because you deserve care that makes sense — and an advocate who sees the person behind the paperwork.
Our approach is simple: clear guidance, compassionate listening, and the belief that understanding is the first step toward empowerment.
founder, third way health
About
Our Story
A new path through healthcare — built on understanding, compassion, and the belief that clarity is care.Third Way Health began with a simple truth: healthcare shouldn’t require a translator.
After years of watching patients feel lost in the system, we set out to create something different — a calm, clear, human-centered way to navigate care.We believe that when patients understand their bills, benefits, and rights, they regain not just confidence, but peace of mind.
Why "Third Way"?
The name comes from the idea that there’s always another path — one that sits between confusion and compliance. The Third Way is the path of understanding: where patients feel informed, empowered, and seen.We don’t just explain the fine print — we walk beside you through it. Our approach blends clarity, compassion, and advocacy to help you make decisions with confidence and peace of mind.

Meet the Founder
Founder & Director of Patient Access and Billing Advocacy.Jessica created Third Way Health after spending over a decade working in healthcare — in both clinical and administrative roles — and seeing how often patients and their families were left to navigate it alone.She is a Certified Revenue Cycle Specialist with 14 years of experience across clinical and administrative billing, coding, patient accounting, HIPAA compliance, authorizations, and appeals. She is an expert in most major insurance plans — including Medicare, Medicare Advantage Plans, Medicaid, Blue Cross Blue Shield, and Priority Health — and has worked in a wide range of healthcare settings including ER, Urgent Care, Neurology, Family Practice, and Physical Therapy.

There’s the system’s way — rigid, confusing, and full of red tape.
There’s the insurance company’s way — designed to delay, deny, and discourage.And caught in the middle is you — the patient, just trying to understand what’s happening and why it has to be this hard.That’s where The Third Way lives — between the two, turning confusion into clarity and giving you space to breathe again.


The Third Way is a patient-centered approach that speaks both languages — the system’s and the insurer’s — and translates them into something human.It’s not about fighting the system; it’s about understanding it, so you can make informed decisions and reclaim control over your care.When you have someone in your corner who knows how it all works, you stop feeling lost — and start feeling capable.
It feels like being seen in a process that usually overlooks you.
It feels like calm in a space that’s built on chaos.
It feels like clarity, compassion, and a way forward that finally makes sense.

You don’t have to keep figuring it out alone.
Keep exploring, or begin with a First Steps Session — a short, supportive call to help you understand what’s going on and what to do next.

Every case is unique.
At Third Way Health, we look beyond the paperwork to understand your story — what happened, what’s confusing, and what support will make a difference. Our goal is simple: to help you move from overwhelmed to informed.

Whenever you’re ready, we're here to walk the next steps with you.
All scheduling is done over the phone — feel free to call to book, or reach out with any questions.
The Open Door Fund exists to make sure cost never stands between someone and the clarity they deserve. When a patient is facing bills they don’t understand, a denial they don’t know how to fight, or a medication stalled by red tape, this fund helps bridge the gap. It keeps the door open for people who need advocacy but can’t afford it right now.

🌿 What the Fund CoversThe Open Door Fund helps qualified patients access any core Third Way Health service, including:• Medical bill reviews
• Benefits checks
• Appeal letters
• Medication and prior authorization support
• Guided Care PlansAll services are provided with the same care, attention, and compassion offered to every client. There are no reduced versions — just real support when it’s needed most.🌱 Who Can ApplyThe fund is application-based and open to patients experiencing financial hardship. Eligibility is determined through a short, income-based form to ensure support reaches the people who truly need it.If you’d like to apply, you can request the form here:
If you’d like to help keep the door open for someone else, you can contribute in any amount. Every dollar goes directly toward patient support — no overhead, no administrative layers, just real, immediate help when someone needs it most.Suggested sponsorships:$25 funds a First Steps Session$85 funds a Medical Bill Review$125 funds an Appeal LetterEven a small contribution can bring clarity, stability, and relief to someone navigating the system alone, helping ensure that support and guidance remain accessible to those who need it most.
Medical bills shouldn’t feel like a second language. We break them down line by line so you can finally understand what you’re being charged for, why it’s showing up, and what to do next.Quick Check – $35
A fast, simple review for one-page bills or single-question concerns. Includes a brief written summary with key takeaways and reassurance on whether anything looks unusual.Basic Review – $85
A detailed review of one bill (up to 5 pages), including a written summary, red flags explained in plain English, and clear recommendations for your next steps. Perfect for labs, office visits, imaging, or recurring bills.Premium Review + Advocacy – $135
For more complex situations or when a conversation is needed. Includes review of up to two bills, a 30-minute consultation, and one provider or insurer follow-up to help resolve discrepancies. Comes with documented findings for future reference.Bundle & Save
3 Basic Reviews – $225
Ideal for patients managing multiple bills or ongoing care.
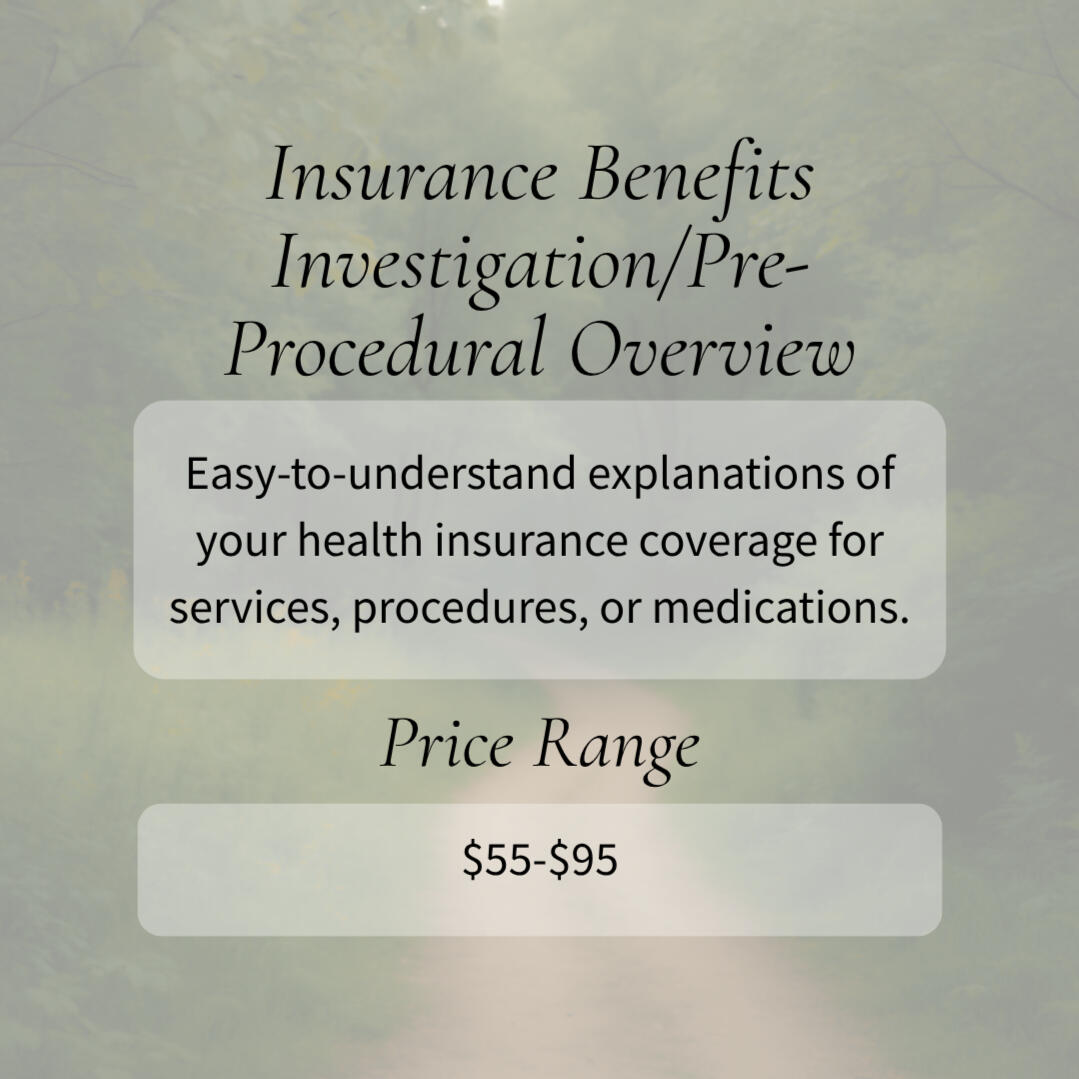
Insurance shouldn’t be confusing. We translate your coverage into human language so you know what’s covered, what isn’t, and what to expect before (or after) a service.Basic Coverage Check – $55
Review of one service, procedure, or medication. Includes a simple, easy-to-understand breakdown of coverage, copays, and your estimated out-of-pocket cost.Premium Deep Dive – $95
A full review of your plan across multiple services, procedures, or medications. You’ll receive a detailed written report, clear explanations of how your benefits apply, and a side-by-side comparison of coverage scenarios.Add-On OptionsOpen Enrollment Support – $75
Compare plan options and understand which one aligns best with your real-life care needs.Pre-Authorization Guidance – $40
We’ll confirm whether prior approval is required, explain the process, and make sure all providers involved (not just the hospital) are in-network.
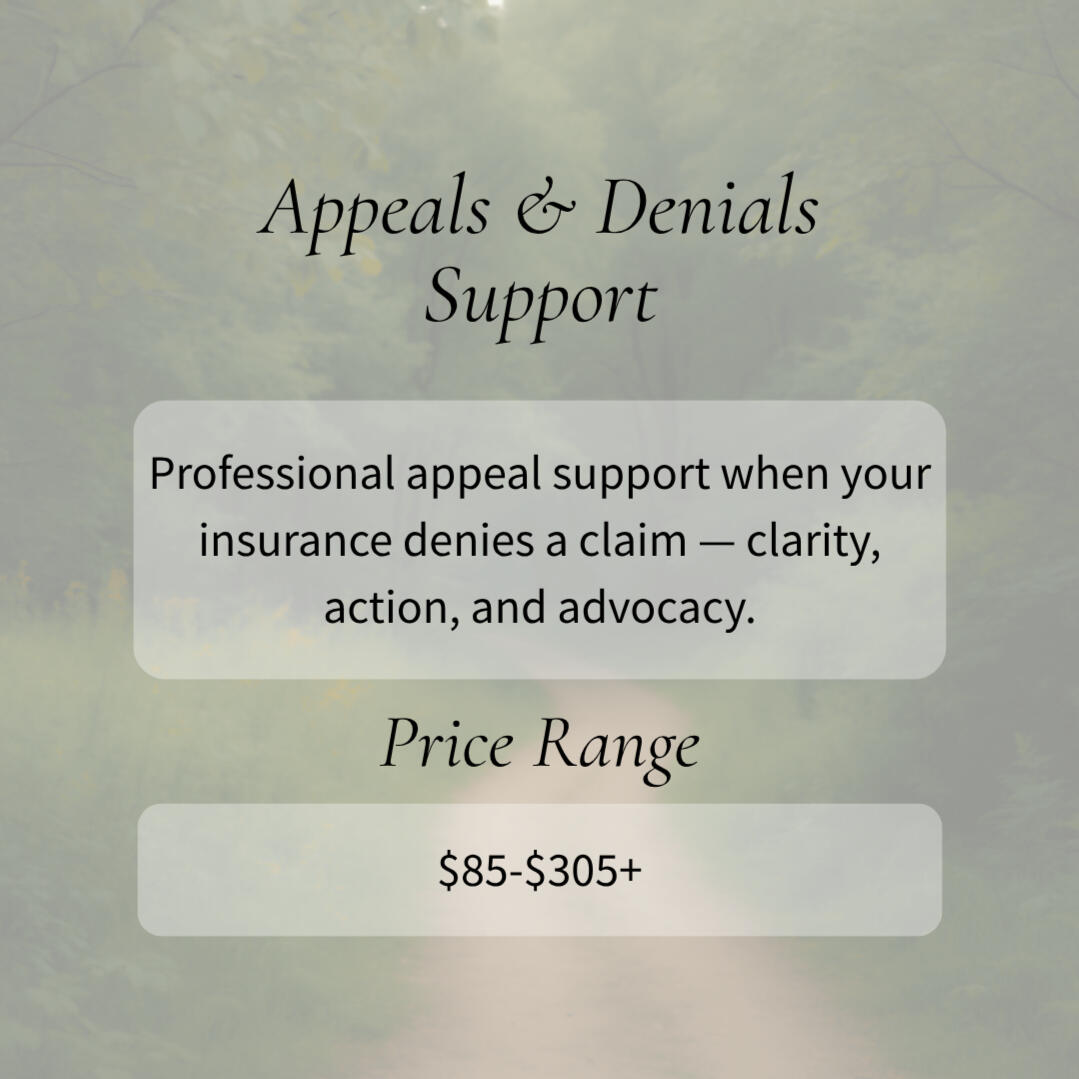
A denial doesn’t have to be the end of the story. We help you understand why it happened and guide you through the process of fighting for fair coverage.DIY Appeal Letter – $85
A professionally drafted, personalized appeal letter tailored to your denial reason, insurer requirements, and supporting documentation. Includes a simple checklist of what to include and how to submit it.Full-Service Appeal – $125 + $90/hr
We manage your appeal from start to finish — drafting, submitting, and tracking it through up to three insurer or provider follow-ups. You’ll receive all correspondence and clear updates as your appeal moves forward.Add-On OptionsExpedited Appeal (+$50) — rush turnaround for time-sensitive denials.Second Appeal Follow-Up – $60 — support if your first appeal is upheld or requires additional documentation.Denial Explanation – $40 — a clear written breakdown of your denial letter and what it means.
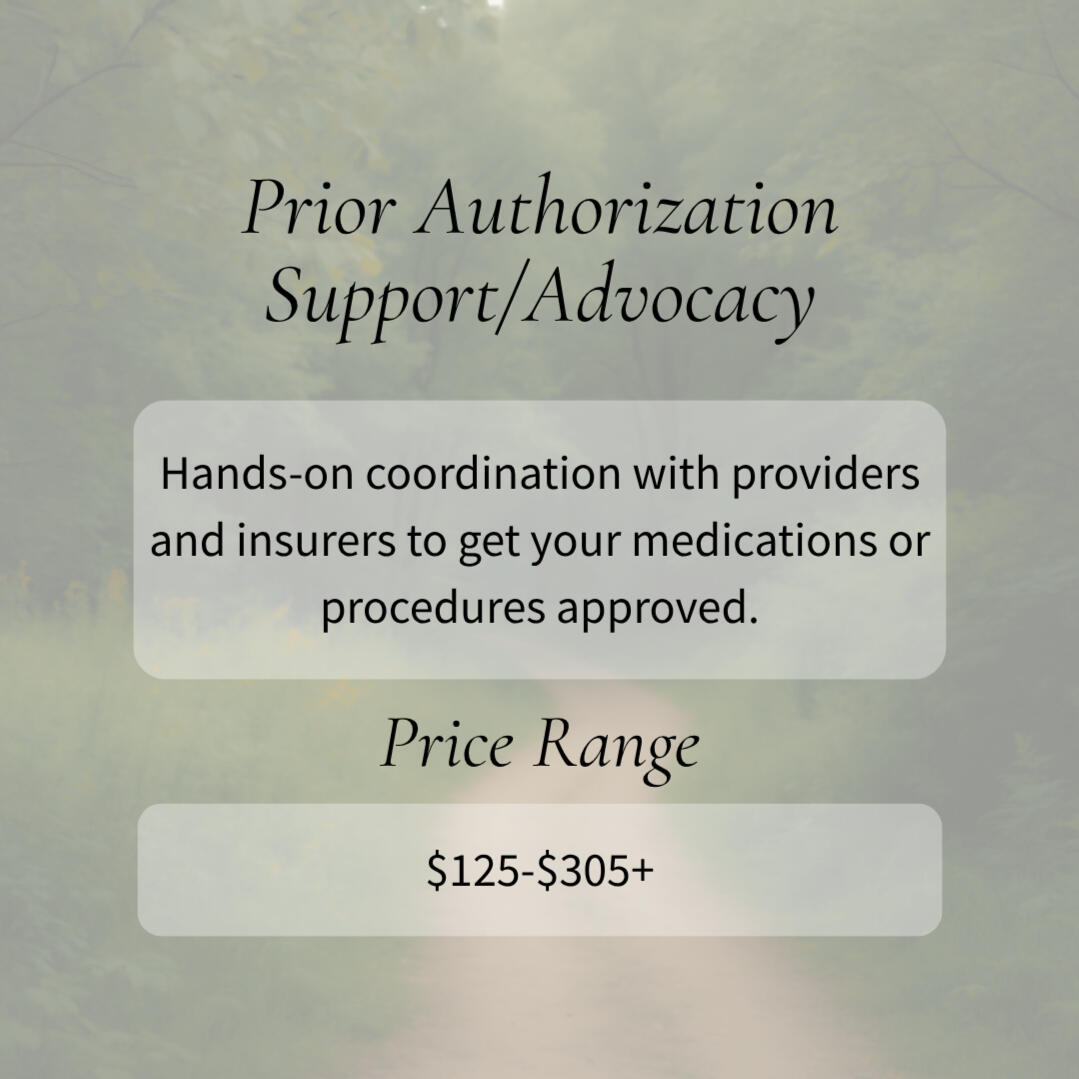
Prior authorizations shouldn’t delay your care. We coordinate between you, your provider, and your insurance company to keep your treatment moving and prevent your request from getting lost in the system.Basic Prior Authorization Assistance – $125
Support for one medication, test, or procedure. We verify benefits, coordinate with your provider’s office, submit the request, and follow up with your insurer to confirm approval status.Full Prior Authorization Coordination – $125 + $90/hr (2-hr min)
For complex, delayed, or previously denied authorizations. Includes gathering documentation, insurer communication, coordination with your provider, and tracking until a final determination is made.Add-On OptionsExpedited Processing (+$50)
Rush handling for urgent medications or time-sensitive treatments.Secondary Appeal Follow-Up – $60
Support if your prior authorization is denied and the next step is a medical necessity appeal.Pharmacy Benefit Deep Dive – $75
Review of formulary tiers, step therapy requirements, alternatives, and manufacturer assistance programs.
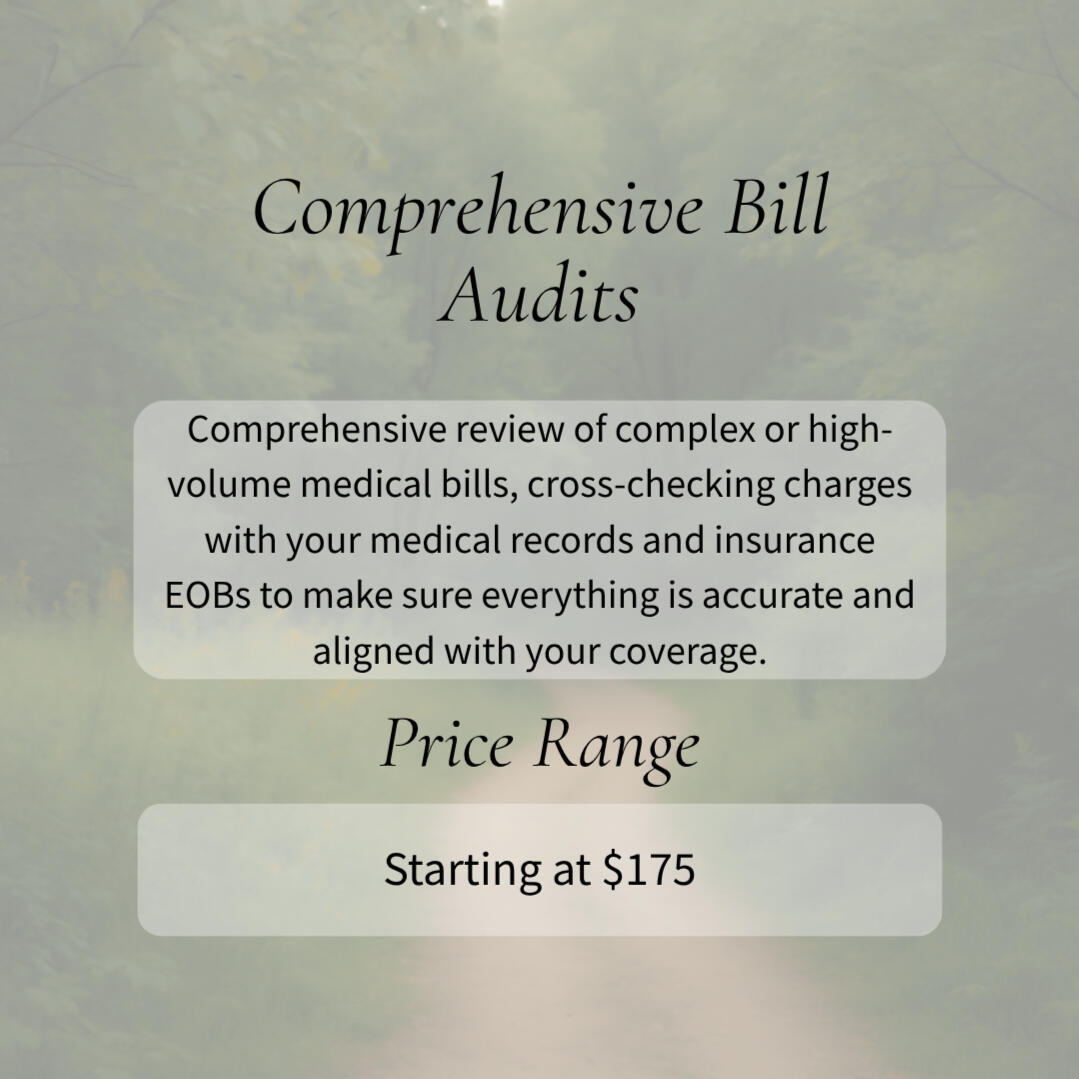
For hospitalizations, ER visits, or large multi-page bills that need a deeper look, we provide a thorough analysis to make sure everything is accurate and aligned with your coverage.Basic Audit – $175
Comprehensive review of complex or high-volume medical bills, cross-checking charges with your medical records and insurance EOBs to ensure accuracy. Includes a written report with findings and clear next steps.Premium Audit + Advocacy – $100/hr (2-hr min)
For 20–50+ page bills or cases involving multiple providers or departments. Includes detailed review, insurer or provider clarification, and follow-up tracking to support corrections or further action.Hospitalization Audit – $250
Flat-rate review for inpatient or ER visits (up to 25 pages), verified against medical records, departmental charges, and EOBs, with a clear summary of what major charges represent.
Navigating healthcare isn’t a one-time task — it’s an ongoing journey.Guided Care Plans offer steady support from someone who already understands your care, your coverage, and your needs. Whether you’re managing chronic conditions, helping an elderly parent or family member, or simply tired of doing it all alone, these plans give you a trusted advocate who can step in quickly, answer questions, and keep everything on track.🧭 The Compass$150 quarterly ($50/month)Guidance when you need it most.For those who like knowing help is just a message away. The Compass plan keeps you connected and supported without ongoing commitments — perfect for individuals or families who handle most things on their own but want the option to reach out when something confusing lands in their inbox.Includes:• Priority email support and responses within 48 hours• Up to one brief question or bill check per month (quick clarifications, “can you take a look at this?” reviews)• 10% discount on full-service offerings (bill reviews, advocacy calls, appeals, etc.)• Client Portal AccessBest for: Patients who want peace of mind and occasional reassurance from a trusted professional.10 Slots Available on a recurring quarterly basis🗺 The Guide$225 quarterly ($75/month)Ongoing support with a familiar face.For those who prefer a more hands-on relationship and value continuity. The Guide plan ensures you have someone ready to interpret, explain, and act — with enough built-in time to tackle new issues as they arise.Includes:• Priority response within 24–48 hours• One included service per quarter (medical bill review, insurance coverage check, or similar)• Unlimited “quick questions” via email or portal message• 10% discount on additional services beyond the included session• Client Portal AccessBest for: Busy professionals, caregivers, retired individuals or families wanting reliable, consistent clarity.Availability: 8 Slots Available on a recurring quarterly basis🌿 The Path$600 quarterly ($200/month)Full-scope, concierge-level advocacy and care coordination.For complex or high-needs cases that benefit from having a dedicated advocate woven directly into the patient’s care journey. The Path plan offers deep, ongoing support — from navigating claims and denials to coordinating across providers when the details matter most.Includes:• Direct phone + email access with same-day or next-day response• Up to three included services per month (bill reviews, benefits breakdown, or active advocacy)• Ongoing monitoring of claims, appeals, and coverage disputes• Attendance at provider appointments (virtual or in-person as applicable)• Priority scheduling and document preparation• 20% discount on additional hourly or specialty services• Client Portal AccessBest for: Individuals with chronic or complex medical needs, or anyone seeking consistent, comprehensive navigation.Availability: 2 Slots Available on a recurring quarterly basis
All Guided Care Plans are paid on a recurring quarterly basis until cancelled.
First Steps Session - $25
The First Steps Session is where new clients start their journey with Third Way Health — a short, focused phone call designed to help you share what’s going on and get clear on what to do next.Whether you’re dealing with a confusing medical bill, an insurance question, a recent denial, or something you just can’t quite make sense of, this session gives us space to talk it through together. We’ll take stock of your situation, outline what information matters most, and identify the best next steps.
There’s no pressure and no sales pitch — just clarity, direction, and support.You’ll walk away with:
• Clarity on what’s happening
• Practical guidance on your next steps
• A recommendation for which service (if any) fits your needs
• A clear outline of what information will be most helpful moving forward
If this feels like the support you’ve been looking for, the next step starts with a call.
Session length, 30 minutes


It’s Okay If It Doesn’t Make Sense.You don’t need to have the right words or perfect paperwork.
You just need a place to start — and someone who understands.Whether you’re lost in the fine print or just feel stuck,
reach out. We’ll find the next step together.

Office Hours:
Monday: 9AM-4PM
Tuesday: 9AM-4PM
Wednesday: 9AM-4PM
Thursday: 9AM-4PM
Friday: 9AM-12PM
Our phone is off daily from 12PM-1PM for lunch
Saturday: Closed
Sunday: ClosedMailing Address:
PO BOX 88
Traverse City, MI 49685Phone:
231-942-4060
Fax:
813-279-6321
General Inquiries:
[email protected]

You know your patients — and their care — better than anyone.
But too often, your day gets swallowed by the other stuff: hours on hold with insurance, deciphering billing errors, chasing authorizations, or trying to explain coverage that even payors can’t explain clearly.At Third Way Health, that’s the work we do — the middle-ground that eats up your time and energy. We handle the details behind the scenes so you and your staff can stay focused on what you do best: caring for your patients.
Bill Review & Explanation — We comb through bills line by line, explaining charges in plain language so patients know exactly what they’re looking at and don’t feel lost in the details.Insurance & Benefit Navigation —We break down what’s covered and what isn’t — in plain, human language. Our job is to guide patients through the space between provider and insurer, making sure the right questions go to the right people so nothing gets lost in the shuffle.Advocacy & Appeals — We help patients navigate denied claims and coordinate directly with their insurers, reducing the questions that end up back at your office. When patients hit a roadblock, we’re the ones who follow up — finding answers, clarifying next steps, and guiding them forward so your team can stay focused on care.Patient Education & Support — We empower patients to ask the right questions, reducing confusion, repeat calls, and stress for your staff. When patients understand what’s happening with their coverage, everyone’s job gets easier — including yours.
• Less administrative burnout for your team•Patients who feel informed, supported, and less overwhelmed• Smoother billing conversations and fewer escalations• Secure, HIPAA-compliant communication and documentation• A trusted extension of your care — focused on clarity, empathy, and understanding